Quick facts about gender-affirming care for minors
Let's combat the misinformation, shall we?
The positive effects of gender-affirming care for transgender and nonbinary people—adolescents and adults—are well-demonstrated in the scientific literature. I’m trans, I have a PhD in public health plus 12 more years of biomedical research experience, the last 6 of them in trans health. Let’s put my science skills to use.
Media coverage, editorials in peer-reviewed journals, and a handful of flawed studies challenge gender-affirming care. Myths, misinformation, and disinformation abound and have directly led to bans on gender-affirming care in 26 states and counting.
This “evidence” comes from fringe medical organizations and scientists, conservative and evangelical donors, and political posturing rather than actual scientific knowledge. (Check out Wuest and Last’s fantastic exploration of this.)
These key science-backed facts about transgender and nonbinary minors counter the pop narrative and disinformation campaigns that are harming children.
General Facts
Proportion of U.S. children and adolescents who identify as transgender: 1-3%
Number of medical interventions on pre-pubescent trans children: 0
Age at which children recognize gender identity: 3 to 6 years
Proportion of children still identifying as trans or nonbinary after 5 years of follow-up: 97.5%
Sources: Coleman 2022, Herman 2022, Mitchel 2022, Hembree 2017, de Vried 2021, Hassan 2024, Doyle 2022, Olson 2022)
Facts about Puberty Blockers (GnRHa)
Proportion of U.S. transgender adolescents who ever used GnRHa: 5%
Minimum number of peer-reviewed studies showing that withholding puberty blockers causes irreversible harm and worse mental health, including suicidality: 6
Sources: Hughes 2025, Ramos 2021, Rew 2021, Schagen 2020, Sorbara 2020, Kreukels 2011, Ghelani 2020
Facts about Gender-Affirming Hormone Therapies (GAHT)
Proportion of U.S. transgender adolescents who used GAHT: 7%
Proportion of transgender adolescents who continued GAHT into adulthood: 98%
Change in average age in years since 2014 at which trans youth start GAHT: 0
Minimum number of systematic reviews published in major peer-reviewed journals that show GnRHa and/or GAHT have positive impacts and low risks of harm on trans adolescents: 11
Sources: Hughes 2025, van der Loos 2022, de Castro 2024, Connolly 2016, Ramos 2021, Chew 2018, Mahfouda 2017, Baker 2021, D’Hoore 2022, Doyle 2023, van Leerdam 2023, Karalexi 2020, Dopp 2024, Brezin 2024
Facts about Gender-Affirming Surgeries in Minors
Cisgender people get gender-affirming care, too. Way more often than trans people do, in fact.
Proportion of all breast reduction surgeries in minors that are performed on cisgender girls: 87%
Number of mastectomies performed in the U.S. on transgender minors aged 13-17 in 2017-2021: 776
Average years younger cisgender girls are when getting breast reduction surgeries vs trans boys getting them: 2-3
Sources: Hassan 2024, Respault 2022
Facts about regret after major life decisions in adulthood
Proponents of the bans talk a lot about regret. But regret for gender-affirming medical care is extremely low—far, far lower than for any other medical procedures and other major life decisions.
Proportion of people who later regret
Transgender gender-affirming surgeries: 1%
Joint replacement surgeries: 30%
Gastric banding surgeries: 20%
Getting tattoos: 16%
Having children: 7%
Sources: Thornton 2024
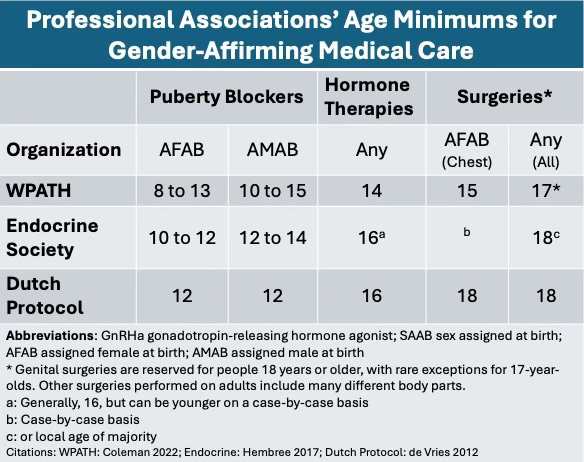
Age Minimums for Gender-Affirming Care
Proponents of bans on care would have you believe that small children are getting operations. This is simply false. The lie is spread to rally anti-transgender sentiment.
In reality, multiple professional organizations have careful, strict guidelines for all gender-affirming medical care. That is especially true for minors.
Medical transition options by age group
Kids < about 11: NONE
Adolescents about 12-15: puberty blockers
Adolescents 16 and older: hormones; chest surgeries for transmasculine/ nonbinary youth
Adults 18+: Hormones, surgeries
Clinical Guidelines Minimum Age Requirements
References
Baker, K. E., Wilson, L. M., Sharma, R., Dukhanin, V., McArthur, K., & Robinson, K. A. (2021). Hormone Therapy, Mental Health, and Quality of Life Among Transgender People: A Systematic Review. J Endocr Soc, 5(4), bvab011.
Brezin, F., Busiah, K., Leroy, C., et al. (2024). Endocrine management of transgender adolescents: Expert consensus of the French Society of Pediatric Endocrinology and diabetology working group. Arch Pediatr. https://doi.org/10.1016/j.arcped.2024.08.003
Chew D, Anderson J, Williams K, et al. (2018). Hormonal Treatment in Young People with Gender Dysphoria: A Systematic Review. Pediatrics, 141(4), e20173742.
Coleman, E., Radix, A. E., Bouman, W. P., et al (2022). Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. International Journal of Transgender Health, 23(sup1), S1-S259. (WPATH)
Connolly MD, Zervos MJ, Barone CJ, et al. (2016). The Mental Health of Transgender Youth: Advances in Understanding. Journal of Adolescent Health, 59(5), 489–495.
De Castro, C., Solerdelcoll, M., Plana, M. T., Halperin, I., Mora, M., Ribera, L., Castelo-Branco, C., Gómez-Gil, E., & Vidal, A. (2024). High persistence in Spanish transgender minors: 18 years of experience of the Gender Identity Unit of Catalonia. Spanish Journal of Psychiatry and Mental Health, 17(1), 35-40.
de Vries AL, Cohen-Kettenis PT. Clinical management of gender dysphoria in children and adolescents: the Dutch approach. J Homosex. 2012;59(3):301-20. (Dutch Protocol)
D'Hoore, L., & T'Sjoen, G. (2022). Gender-affirming hormone therapy: An updated literature review with an eye on the future. J Intern Med,291(5), 574-592. Mental Health, and Quality of Life Among Transgender People: A Systematic Review. J Endocr Soc, 5(4), bvab011.
Dhanani LY, Totton RR. Have You Heard the News? The Effects of Exposure to News About Recent Transgender Legislation on Transgender Youth and Young Adults. Sex Res Social Policy. Apr 5 2023:1-15. doi:10.1007/s13178-023-00810-6
Dopp, A. R., Peipert, A., Buss, J., de Jesus-Romera, R., Palmer, K., & Lorenzo-Luaces, L. (2024). Interventions for Gender Dysphoria and Related Health Problems in Transgender and Gender Expansive Youth: A Systematic Review of Benefits and Risks to Inform Practice, Policy, and Research. Doyle, D. M. (2022). Transgender identity: Development, management and affirmation. Curr Opin Psychol, 48, 101467.
Doyle, D. M., Lewis, T. O. G., & Barreto, M. (2023). A systematic review of psychosocial functioning changes after gender-affirming hormone therapy among transgender people. Nat Hum Behav, 7(8), 1320-1331.
Ghelani, R., Lim, C., Brain, C., Fewtrell, M., & Butler, G. (2020). Sudden sex hormone withdrawal and the effects on body composition in late pubertal adolescents with gender dysphoria. J PediatrEndocrinol Metab, 33(1), 107-112.
Hassan, B., Zeitouni, F., Ascha, M., Sanders, R., Berger, Z., Fields, E., & Liang, F. (2024). Breast Surgery in Adolescents: Cisgender Breast Reduction Versus Transgender and Nonbinary Chest Masculinization. Ann Plast Surg, 93(2), 194-199.
Hembree WC, Cohen-Kettenis PT, Gooren L, et al. (2017). Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline, Journal of Clinical Endocrinology and Metabolism. (Endocrine Society)
Herman JL, Flores AR, O’Neill KK. (2022). How Many Adults and Youth Identify as Transgender in the United States? Los Angeles: The Williams Institute. https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/
Hughes, L. D., Charlton, B. M., Berzansky, I., & Corman, J. D. (2025). Gender-Affirming Medications Among Transgender Adolescents in the US, 2018-2022. JAMA Pediatr.
Karalexi, M. A., Georgakis, M. K., Dimitriou, N. G., Vichos, T., Katsimpris, A., Petridou, E. T., & Papadopoulos, F. C. (2020). Gender-affirming hormone treatment and cognitive function in transgender young adults: a systematic review and meta-analysis. Psychoneuroendocrinology, 119, 104721.
Kreukels, B. P., & Cohen-Kettenis, P. T. (2011). Puberty suppression in gender identity disorder: the Amsterdam experience. Nat Rev Endocrinol, 7(8), 466-472.
Mahfouda S, Moore JK, Siafarikas A, et al. (2017). Puberty Suppression in Transgender Children and Adolescents. Lancet Diabetes & Endocrinology, 5(10), 816–826.
Mitchell HK, Keim G, Apple DE, et al. (2022). Prevalence of Gender Dysphoria and Suicidality and Self-Harm in a National Database of Paediatric Inpatients in the USA: a Population-based, Serial Cross-Sectional Study. Lancet Child and Adolescent Health, 6(12), 876–884.
Movement Advancement Project. 2025. "Equality Maps: Bans on Best Practice Medical Care for Transgender Youth." https://www.mapresearch.org/equality-maps/healthcare/youth_medical_care_bans. Accessed April 9, 2025.
Olson, K. R., Durwood, L., Horton, R., Gallagher, N. M., & Devor, A. (2022). Gender Identity 5 Years After Social Transition. Pediatrics, 150(2).
Ramos GGF, Mengai ACS, Daltro CAT, et al. (2021). Systematic Review: Puberty Suppression with GnRH Analogues in Adolescents with Gender Incongruity. Journal of Endocrinological Investigation, 44(6), 1151–1158.
Respaut R, Terhune C. (Oct 6, 2022). Putting numbers on the rise in children seeking gender care. https://www.reuters.com/investigates/special-report/usa-transyouth-data/ Accessed Jan 2024.
Rew, L., Young, C. C., Monge, M., & Bogucka, R. (2021). Review: Puberty blockers for transgender and gender diverse youth-a critical review of the literature. Child Adolesc Ment Health,26(1), 3-14.
Schagen, S. E. E., Wouters, F. M., Cohen-Kettenis, P. T., Gooren, L. J., & Hannema, S. E. (2020). Bone Development in Transgender Adolescents Treated With GnRH Analogues and Subsequent Gender-Affirming Hormones. J Clin Endocrinol Metab, 105(12), e4252-4263.
Sorbara, J. C., Chiniara, L. N., Thompson, S., & Palmert, M. R. (2020). Mental Health and Timing of Gender-Affirming Care. Pediatrics,146(4).
Thornton SM, Edalatpour A, Gast KM. A systematic review of patient regret after surgery- A common phenomenon in many specialties but rare within gender-affirmation surgery. The American Journal of Surgery. 2024;doi:10.1016/j.amjsurg.2024.04.021
van Leerdam, T. R., Zajac, J. D., & Cheung, A. S. (2023). The Effect of Gender-Affirming Hormones on Gender Dysphoria, Quality of Life, and Psychological Functioning in Transgender Individuals: A Systematic Review. Transgend Health, 8(1), 6-21.
van der Loos MATC, Hannema SE, Klink DT, et al. (2022). Continuation of Gender-Affirming Hormones in Transgender People Starting Puberty Suppression in Adolescence: A Cohort Study in the Netherlands. Lancet Child and Adolescent Health, 6(12), 869–875.
Wiepjes, C. M., Nota, N. M., de Blok, C. J. M., Klaver, M., de Vries, A. L. C., Wensing-Kruger, S. A., de Jongh, R. T., Bouman, M. B., Steensma, T. D., Cohen-Kettenis, P., Gooren, L. J. G., Kreukels, B. P. C., & den Heijer, M. (2018). The Amsterdam Cohort of Gender Dysphoria Study (1972-2015): Trends in Prevalence, Treatment, and Regrets. J Sex Med,15(4), 582-590.




Thank you soooooo much for this, and all the time and work you put into it. It’s priceless for advocacy of trans youth and deeply appreciated.
I was 15 when I first started HRT! It is fully dependent on what stage of puberty you are in! I was at my last stage.