Gender transition isn't what you think it is: Part 4a: Hormonal Transition
A series on psychological, social, legal, and medical transition & what it means to be trans
Read Part 1: Psychological Transition, Part 2: Social Transition, and Part 3: Legal Transition.
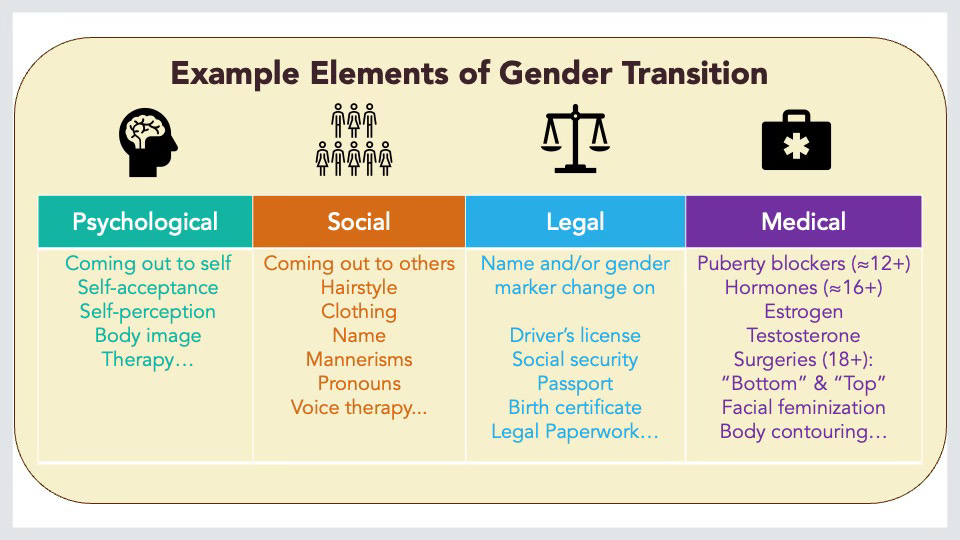
Part 4 is finally here! Well, Part 4a. I find it helpful to break down gender transition into several major categories: psychological, social, legal, and medical.
Now that I’m writing the medical section, I see how long it is, so I’m splitting it further into a) hormones and b) surgeries and other medical procedures.
First, let’s talk about medical transition overall.
In the popular discourse, medical transition is what people commonly think of when we talk about gender transition and transgender people in general. But many transgender and nonbinary people never medically transition.
Others do some types of medical transition and not others. Some have transition goals that they never meet. These are for a lot of reasons:
The options aren’t available where they live.
The options aren’t legal where they live.
They can’t access the services that are available because
Lack of insurance that covers this care
Lack of financial resources for copays, transport, etc.
Distance to care is too much of a time and money burden
Inability to take time off work
Lack of access to mental health providers who will write supporting letters
Lack of friends or family who can care for them post-surgery.
The available options won’t satisfy their transition goals.
This is true about masculinizing gential surgeries for a lot of people. The options aren’t good enough to go through the whole multi-stage process.
They don’t want/need to. Hormones and surgeries are not for everyone.
Transgender health care is safe.
Before I get into details, let’s talk about the safety of transgender medical care, risks, and benefits. Disinformation (deliberately wrong and misleading information) abounds about transgender health care; this is all part of a larger goal to erase and eradicate transness that the current administration is attempting to bring to horrifying fruition now in the US.
The anti-trans rhetoric stokes people’s fears and concerns, especially for children and young people. Who doesn’t want to protect their children? I’m a parent. I get it.
This is a calculated tactic. When we are afraid, we cannot think clearly and logically, so when the anti-trans folks hand out an easy solution (banning trans care for youth, for example), people agree quickly because it helps their fear go away. This is normal, natural, and human. It applies to educated and intelligent people, too; we all make decisions based on our emotions far more than we realize.
The truth is that every single hormonal regimen and medical procedure in transgender health care was first used on cisgender people. These procedures are still provided to cisgender people, even in states where the governments have barred trans people from accessing the exact same procedures.
They are safe. The benefits well outweigh the risks. I’m elbow-deep in the biomedical literature on this—I’m an epidemiologist—and can provide references and explanations for days. But I’ll leave that literature for later. If a reader has any specific questions, do ask!
We have broad categories within medical transition: hormones, surgeries, and other medical procedures.
Hormones: puberty blockers, masculinizing hormones (i.e., testosterone), and feminizing hormones (i.e., estrogen).
Surgeries: a large number of surgeries on various body parts: the head and face, chest, abdomen, hips, and pelvic area.
Other medical procedures: a grab bag of other things, like hair removal and voice therapy
Let’s talk hormones.
Hormones
I’m breaking hormones down into three main regimens: puberty blockers, feminizing hormones, and masculinizing hormones.
Puberty Blockers
Puberty blockers pause and postpone puberty in preteens and teens.
These medications may also be called
Hormone blockers
Puberty suppression medications
Puberty inhibitors
Gonadotropin-releasing hormone agonists (GnRH)
Specific names like histerlin acetate and leuprolide acetate
As I said earlier, these are used for cisgender children, too. In those cases, they are prescribed when children start puberty way too early. Once they are old enough to start puberty, they stop taking the blockers, and their puberty resumes like usual. Even if they did have some risks to them, you must weigh those risks against the benefits of not having a period at age 6, ya know?
All the medical organizations1 that provide guidelines for transgender medical care use the Tanner Stage 2 cut-off. Stage 2 is when physical changes just start to become visible. That’s roughly ages 9-12 for people assigned female at birth, 11-13 for people assigned male at birth, and it depends on a lot of factors for intersex people.
Since the function is to pause puberty, pre-pubertal children do not need puberty blockers. Trans children who have not yet reached puberty (Tanner Stage 2, specifically) do not get any hormones, surgeries, or other transition-related medical procedures.
Our society labels estrogen and testosterone as “sex hormones,” and we associate estrogen with females and testosterone with men. But these hormones are in all bodies in varying amounts. Ovaries produce both estrogen and testosterone. Testes produce testosterone, and then the body converts some of that T into estrogen. Several body systems use these hormones, and all bodies need both.
That said, our puberties and secondary sex characteristics are driven primarily by one or the other.
Feminizing
Estrogens (and variations of it) have a feminizing effect on bodies, whether that body was assigned male or female at birth, whether that body is 18 or 78. Skin softens, body hair growth slows, breasts develop, fat distribution on the body moves to the hips, etc.
Doctors also prescribe anti-androgens, which suppress testosterone. If the person has her gonads removed, that means the body isn’t producing testosterone like before, so they can stop taking anti-androgens and may need to adjust the dose of estrogens. But that’s the job of the health care providers to figure out through careful lab monitoring.
These hormone regimens are not birth control! Some trans women still produce viable sperm and can impregnate. Some go off the hormones in order to have a planned pregnancy with a partner.
Masculinizing
Testosterone has masculinizing effects on bodies, whether that body was assigned male or female at birth, whether that body is 18 or 78. The right amount of testosterone causes the body to go through puberty, with the accompanying hair, horniness, hunger, body odor, voice cracking, muscle growth, etc. How much facial and body hair you get and whether or not you go bald depends on genetics.
Usually, menses stop. However, T is not effective birth control! Off T, fertility can resume. These days, lots of trans men stop T so they can carry pregnancies, and they do so healthily.
One size does not fit all
In the past (and still in some practices), there’s a one-size-fits-all checklist of medical transition (“transnormativity”). But these days, we individualize care much more. Think cafeteria style or a smorgasbord. Hormones can be prescribed in lower or higher doses, for example. Some people take a microdose of T because they want a slower effect to achieve a more androgynous look rather than a masculine one. Others may want just enough to stop their menses. Others can’t wait to get the full dose in their bodies the second the provider clears them.
This is a huge subject. I could write so much more. I’ll save it for later posts. In the meantime, like, share, restack, and subscribe! Feel free to ask questions.
World Professional Association for Transgender Health (WPATH) Standards of Care 8; The Endocrine Society; UCSF Center of Excellence for Transgender Health