Gender transition isn't what you think it is: Part 4b, Surgical Transition
A series on psychological, social, legal, and medical transition
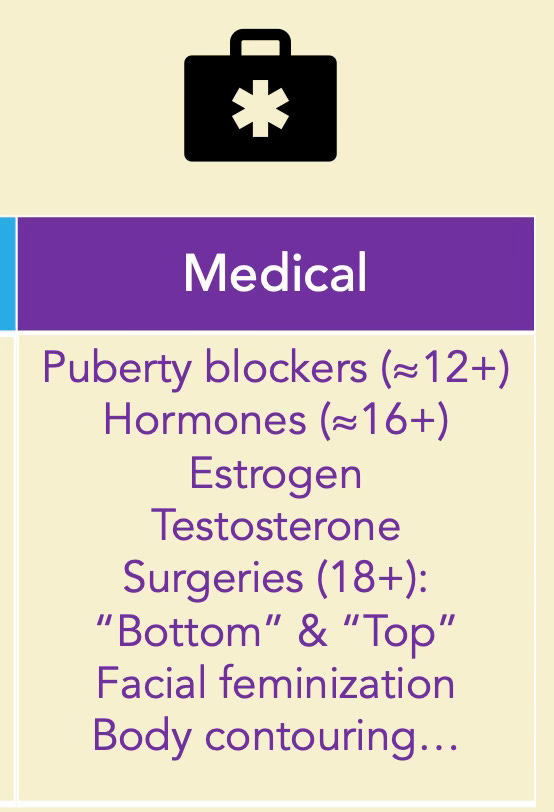
For this series, we break down gender transition into several major categories: psychological, social, legal, and medical. We can further break down the medical category into a) hormones and b) surgeries and other procedures.
Let me make clear upfront: Surgical procedures on genital organs for gender affirmation are reserved for adults. Exceptions are very rare.1
A Preface about Private Parts
In the first post in this series, I asked what first comes to mind when you hear transgender or gender transition. In my experience, people’s brains jump to genitals and surgery, whether or not they say it out loud.
A lot of trans people, myself included, have had family, friends, and even strangers ask us questions like these:
Are you gonna get the surgery?
Are you going, like, all the way?
Have you fully transitioned?
I get it. Curiosity is normal. The same questions often pop into my head when I meet a trans person. But these questions boil down to “What’s in your pants?” or more explicitly, “What do your genitals look like?”
Which, if you think about it, is impolite and inappropriate. That information is personal and private. Only two types of people need to know: medical providers and sexual partners. (And not even all of them need to know!)
Before you ask any trans/nonbinary person about their personal medical history, think about what you are asking and why. Even among trans folx, I find that people preface with, “May I ask you a medical question?” or “Do you mind me asking a question about your transition history?”
That is, ask for consent first. And take no for an answer.
I’m pretty open about my transition, so I’m comfortable writing this newsletter, giving webinars, and answering people’s questions. But if I get the “what’s in your pants?” variety of questions, I’ll educate about trans-related surgeries in general.
If you’re genuinely curious, ask for a recommendation of a book, video, or other media where you can learn more. This preserves the trans person’s privacy and doesn’t put the burden on them of educating you. You are just one person, but they get the question a lot.
I highly recommend these books and authors. Both are trans themselves and educate on trans issues professionally.
He/She/They by Schuyler Bailar, for general knowledge
My Child Is Trans, Now What? by Ben Greene, for parents and caregivers/relatives of trans/nonbinary kids (even if they are grown now).
As I wrote in the Hormones post, barriers prevent people from accessing care, and many trans people never medically transition for a lot of reasons. Most do some things, but not all. Each person has their transition goals; there is not an end point everyone is trying to reach.
In fact, less than 5% of trans men/masculine people get any gential surgery (“phallo” or “meta,” see below), and less than half want it in the future.2
Even if someone does not medically transition or they start then stop taking hormones, they are still trans/nonbinary if they feel they are. Remember, gender identity is fundamentally an internal understanding of oneself.
All that said, medical transition is necessary and life-saving for trans/nonbinary people who need it. So, let’s get to the surgical aspects of transition.
Disclaimer: This page does not provide medical advice or information. Check the links to actual medical sites below.
Surgeries
Lingo
When it comes to surgical transition, I only ever use the terms “The Surgery” or “sex-change operation” ironically, and many trans people find those terms offensive. Even “surgical transition” is a more academic/data analysis term.
In trans lingo, we use the terms “top surgery” and “bottom surgery” (or “lower surgery”), but even these are broad categories of several surgeries. Multiple surgeries can be performed on many different body parts.
Since many body parts can cause trans/nonbinary people discomfort, even hearing or saying the words for those parts can be difficult. (I’ve always despised the word breasts.) To overcome this, the community has invented all sorts of alternative terms—many of them silly. We’ve also made fun terms for surgeries. For example, we’ve got these for trans man/masculine/nonbinary:
Misterectomy
Duderous
Brovaries
Teet yeet
Teetus deletus
Chesticles
(Trans people get to have fun, too.)
Top Surgeries
“Top surgery” usually refers to procedures performed on the chest and breasts. In cisgender people, these surgeries are called breast augmentation (a “boob job”), breast reduction (making the breasts smaller or flatter), and double mastectomy (removing both breasts). All gender-affirming medical care is also performed on cisgender people.
For trans women and other transfeminine people, hormone therapy causes breast growth. Genetics matter here, and some people get breast augmentation to achieve a larger size.
Many trans men, transmasculine people, and nonbinary people get either a breast reduction or a double mastectomy. But those terms can cause gender dysphoria, as they call attention to body parts that feel uncomfortable, foreign, or wrong (as they did for me). Instead, we say top surgery, double incision, or chest masculinization. A variety of surgeries and surgical techniques can achieve the flat-chest look.
I got a double incision myself in 2019. I wear my scars proudly—the mark of a self-made man. I’ll share more about how I felt about my pre-surgery chest in other posts. Suffice it to say for now, the last time I was in an ob-gyn office for my “annual,” the mere mention of a breast exam sent me into a panic attack. Even using the word breast in this post is difficult for me; I have to remind myself that trans women feel gender euphoria about their breasts.
Some surgeons will perform chest masculinization surgeries on trans youth ages 14 to 17 years old with parental permission and mental health evaluation. About 7 times more cisgender teenage girls get breast reduction surgeries than transgender teenage boys. Cisgender girls get these surgeries on average two years younger than trans boys.3
Bottom Surgeries
Bottom surgeries include surgeries on genitals, yes, but also other abdominal, pelvic, and reproductive system surgeries. These are done in adults.
For trans women/feminine/nonbinary people:
Vaginoplasty
Orchiectomy, Penectomy
For trans men/masculine/nonbinary people:
Phalloplasty, aka phallo
This usually requires 4 or more surgeries over a couple of years & a whole lot of hair removal first
Metoidioplasty, aka meta
Hysterectomy
Salpingo-oophorectomy (removal of fallopian tubes and ovaries)
Non-genital/reproductive system Procedures
Body contouring procedures for a more masculine or feminine look
Facial surgeries for a more masculine or feminine look
Changes to the forehead, jawline, nose, Adam’s apple, cheeks
Hairline changes; hair transplants
Chondrolaryngoplasty/Tracheal shaving (to make the Adam’s apple less prominent)
Hair removal
From face and body for a more feminine look
From forearm in preparation for phalloplasty
Voice therapies (including surgery)
Some Numbers
Trans medical care guidelines state that bottom (genital) surgeries are reserved for people 18 years and older.
Top surgeries can be performed on teenagers on a case-by-case basis and with permission from parents, medical provider, surgeon, and mental health provider.
Despite the outsized news and political coverage gender-affirming care gets, surgeries are actually quite rare. A 2024 study published in the Journal of the American Medical Association (JAMA), written by Dai and colleagues4 searched national medical claims data for instances of gender-affirming surgeries.
They found these rates of surgeries by age group:
Adults 18+: 0.0053%
15-17 year olds: 0.0021%
13-14 year olds: 0.0001%
12 years old and younger: 0. Zero. Zilch.
But hold up! These are the numbers in all people, transgender and cisgender. Almost all of those surgeries were chest-related and in cisgender men! Cisgender boys and men can develop gynecomastia—breast growth.
Most of the surgeries in the bulleted statistics were breast reductions in cisgender men.
Surgical transition has been politicized and weaponized, especially around kids, so this is a dicey topic. I am writing a separate post about what gender-affirming care and gender transition are and aren’t for kids (spoiler: not surgery).
Links to medical information on trans surgeries & other care:
Johns Hopkins Center for Transgender and Gender Expansive Health
Mayo Clinic Transgender and Intersex Speciality Care Clinic
UCSF Guidelines for Primary and Gender-Affirming Care for Transgender and Gender Nonbinary People
WPATH Guidelines (Standards of Care 8)
https://www.reuters.com/investigates/special-report/usa-transyouth-data/
Nolan IT, Kuhner CJ, Dy GW. Demographic and temporal trends in transgender identities and gender confirming surgery. Transl Androl Urol. 2019 Jun;8(3):184-190.
Hassan B, Zeitouni F, Ascha M, et al. (2024). Breast Surgery in Adolescents: Cisgender Breast Reduction Versus Transgender and Nonbinary Chest Masculinization. Annals of Plastic Surgery.
Dai DD, Charlton BM, Boskey ER, et al. (2024). Prevalence of Gender-Affirming Surgical Procedures Among Minors and Adults in the U.S. JAMA.




Thank you for explaining this so thoroughly. Well written and clear.